My Psychiatric Treatment Is Not Working – Why?
- Home
- Blog
An Outmoded Model of Care
Dear Reader,
Have you or someone you know been navigating the complex world of psychiatric treatment, only to find yourselves in the same, uncharted waters of distress as when you began? It is not just you. This sense of disillusionment is not unfounded but a reflection of a larger, systemic issue within the realm of mental health care. It is understandable to feel cynical, hopeless, or even resigned after rounds of treatment that promise much but deliver little in terms of genuine, lasting recovery. This is the reality for many navigating the psychiatric care system—a system entrenched in models of care that, while groundbreaking in their inception, now falter under the nuanced demands of individual mental health complexities.
The heart of the matter lies in the traditional approach to psychiatric treatment, which is fundamentally rooted in a one-size-fits-all, population-based science. This model, while it has its merits, often falls short because it fails to consider the unique, multifaceted nature of each individual's mental health. The result? A treatment resistance that leaves countless individuals battling their demons without relief, as the core “root cause” issues go unaddressed.
With astonishing advances in the field of personal genomics, gut microbiome science, longevity, and molecular biology and cellular health, it is time for a novel approach - Holistic Psychiatry.
The Need for a Paradigm Shift
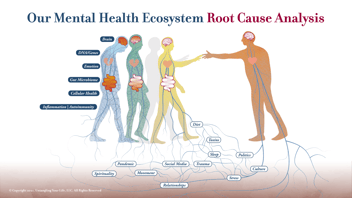
What is urgently needed is not another “trial-and-error" approach to the prescription pad, but a paradigm shift towards a root cause analysis approach in psychiatric care. This means moving away from the surface-level symptom management to a deeper exploration of the underlying factors contributing to mental health conditions. It is about understanding that the mind and our emotional life do not exist in isolation but are intrinsically linked to the body's complex biological systems. Including the relationships between its 30 trillion human cells, 39 trillion gut microbes, and the 100 trillion atoms and billions of molecules inside each cell! These complex systems are addressed and treated by a new paradigm that I have named Root Cause Psychiatry™.
Unpacking the Layers: Beyond Symptoms to Root Causes
- Genetic Vulnerabilities: Our genes can predispose us to various mental health conditions, but without the right (or wrong) environmental triggers, known as “epigenetic influences,” these predispositions may never become manifested as psychiatric conditions. Identifying these genetic vulnerabilities through Genetic Testing can guide more personalized, effective treatment strategies including the targeted use of supplements, nutrients, and/or medication to “turn on” health-promoting genes and “turn-off” genes that promote mental health symptoms.
- Gut Microbiome Problems: The gut-brain axis is a critical pathway that can lead to mental wellness or major mental illness, with an imbalanced gut microbiome contributing to mental health issues through inflammation, dysbiosis, maldigestion and malabsorption, short chain fatty acid deficiencies and other mechanisms. Addressing gut health can be a pivotal step in treating psychiatric disorders.
- Cellular Health Concerns: At the cellular level, dysfunction can lead to a myriad of problems, including those affecting mental health. This includes mitochondrial dysfunction, oxidative stress causing free radicals, and more, highlighting the need for treatments that restore cellular health.
- Metabolic Problems: Metabolic dysfunctions, such as insulin resistance and poor glucose metabolism, can have profound impacts on brain health and function, underscoring the need for metabolic considerations in psychiatric treatment. Insulin resistance is a primary cause of mitochondrial dysfunction, as it limits the availability of glucose to be used by brain mitochondria to create energy. The brain is a huge energy consumer - it weighs about 3% of the body’s mass but must produce 20 – 25% of the entire energy produced in the body to function normally.
- Hormone Imbalances: Hormones play a crucial role in regulating genes, mood, and one’s emotions. Imbalances can lead to significant mental health challenges, making hormone regulation a key area for treatment focus. The classic examples of this are menopause and andropause (low levels of testosterone).
- Immune System Dysregulation: The link between inflammation and mental health is well-documented. An overactive, underactive, or poorly regulated immune system can lead to psychiatric symptoms, suggesting treatments should also aim to balance immune function. Not uncommonly, immunologic medication is combined with psychiatric medications like antidepressants.
- The Role of Infectious Diseases: Certain infections can impact brain function and contribute to mental health issues, requiring treatments that address these underlying infections. This includes conditions such as Long COVID, PANDAS/PANS in children, and numerous other infectious diseases.
- Toxins: Exposure to environmental toxins can have deleterious effects on mental health. Identifying and reducing exposure to these toxins is crucial for some individuals' psychiatric treatment. And identifying genes that reduce one’s ability to remove toxins such as heavy metals and pesticides from the body, and modifying the expression of genes to accelerate detoxification, can be an important strategy once toxins are identified through laboratory testing.
Moving Forward: A Call to Action
This is not just about challenging the status quo; it is about embracing a more holistic, integrative approach to mental health care that honors the complexity of the human experience. It is time to shift our focus from purely symptom management to a more comprehensive, root cause analysis that considers genetic, biochemical, and environmental factors.
But where do you begin? Start by advocating for yourself or your loved ones. Seek out professionals who are willing to look beyond the surface, who understand the intricate dance between body and mind, and who are equipped to address the root causes of mental health issues.
You Are Not Alone
If you have felt let down by traditional psychiatric treatments, know that there is hope. There is a growing movement towards integrative mental health care that seeks to address the individual as a whole—mind, body, and spirit.
Book Your No-Cost Consultation
Intrigued by the possibility of a different approach to psychiatric care? Ready to explore how addressing root causes could change your path to mental wellness? We invite you to book a no-cost consultation with our team. Let us discover together how a personalized, integrative approach to mental health can offer not just hope, but real, sustainable healing.
Together, we can chart a new course towards mental health and well-being, one that acknowledges the intricate web of factors influencing our psychiatric health. It is time to move beyond the limitations of traditional treatment models and embrace a future where comprehensive root cause analysis paves the way to genuine recovery and thriving mental health. Book your consultation today and take the first step towards a life defined not by your struggles, but by your strength and resilience in overcoming them.
.png?width=144&height=144&name=Untitled%20design%20(34).png)