Is Your Gut-Brain Axis Making You Moody?
- Home
- Blog

Reader, where does your sense of “Self” reside? It’s easy to feel that our mind, our very conscious awareness, lies in the brain alone. However, our language often points to a different–and more accurate–truth. When we are in love, we describe “butterflies in our stomach.” When we are worried, we describe an uneasy “gut feeling.” When we are about to make a big decision, our loved ones tell us to “trust your gut.”
Why is it, if we are prone to believing that our ultimate command center lies in our skull, that we attribute so many of our emotional states to somewhere entirely different?
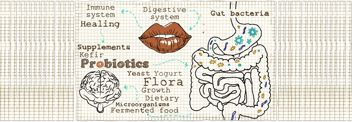
Almost 2500 years ago, Hippocrates said, “All health begins in the gut.” We’ve known for some time that eating healthy foods is a general tonic for the body and brain–but new research is showing another reason to pay attention to what we feed ourselves. Our microbiome, as it turns out, may have a greater impact on our emotional state than we ever thought. In fact, thanks to new research on our Gut-Brain Axis, we are learning critical information about how our microbiome and our brains speak to each other constantly throughout the day, impacting our moods and so much more.
How Does the Gut-Brain Axis Really Work?
Defined as a “bi-directional and regulatory system involving the brain, central nervous system, and… the gut”, the Gut-Brain Axis is a system that connects two critical messaging centers in our body.
The Axis sends messages in three ways: through our vagus nerve, which connects our brain and gut together through a network of nerves; through circulating immune cells that are “educated in the gut and then travel to the brain”; and through metabolites produced in the gut that circulate to the brain to impact our mood, cognition and behavior.
While we frequently think of mood-regulating neurotransmitters as being manufactured in the brain, bacteria in the gut can also produce these chemicals and secrete them out to our bodies to regulate or deregulate our moods. As just one example, lactobacillus can secrete acetylcholine, a neurotransmitter that regulates mood, learning, memory and attention, and can also increase BDNF–a key neurotransmitter involved in stress resilience, mood regulation, and more. In fact, 95% of all the serotonin and 50% of all the dopamine in our bodies is produced in our gut!
Diagnostic tests can help you and your doctor determine the state of your microbiome health, which can in turn help you understand how to modify your microbiome to improve your mental health. By targeting your microbiome through interventions like nutritional psychiatry, you can use the Gut-Brain Axis to your advantage, using nutrition and lifestyle interventions to influence the messages being passed between the two.
Don’t Let your Gut-Brain Axis Make Your Mental Health Worse
The feedback loop between your brain and your gut is an overwhelmingly positive thing to understand, and to take advantage of. But it’s just as important to understand the consequences that can occur when we take that feedback loop for granted.
Scientific research has shown that changes in our gut can contribute to mental illness, like depression. But Depression itself can also induce further modification of our gut microbiota, which can lead to more severe depression. As we frequently point out in this blog, knowledge is power, and the more you understand how you “feed your gut” (for good or for ill), the better you can take care of this important feedback loop–and feed your Gut-Brain Axis the right way.
.png?width=144&height=144&name=Untitled%20design%20(34).png)