Can a Simple Test Help You Recover from Long COVID Brain Fog?
- Home
- Blog

Long COVID can lead to depression, brain fog, cognitive impairment, anxiety, PTSD, and even psychosis—and it can also lead to autoimmune diseases that can further disrupt your mental and physical health.
In this blog you will learn:
- The connection between infectious diseases and psychiatric symptoms
- How COVID can lead to autoimmunity
- The origins of long COVID autoimmunity
- Why anti-brain antibodies are a root cause of psychiatric symptoms
- How the Cunningham Panel diagnoses brain autoimmunity
- How Potomac Psychiatry uses the Cunningham Panel to help patients with long COVID
Long COVID and other Infectious Diseases can Cause Psychiatric Symptoms and Brain Fog
My Dear Reader: Have you had your fill of the daily newsfeed about “the latest variant” of COVID? I know I have. It feels like a continuing onslaught. The good news is that, in contrast to many of those infected earlier by the Delta and Wuhan variants, most folks who get infected with Omicron subvariants have milder symptoms and a shorter course of illness. But while the life-threatening nature of this “global viral bully” appears to be largely behind us, the impacts of long COVID continue to bedevil the lives of many.
In the earlier phases of the pandemic, up to 30% of those infected developed this debilitating syndrome. In the Omicron Era, that percentage appears to have dropped to 5-15%. This is a good sign—yet far too many individuals are still affected by long COVID every day, with no sign of relief in sight.
Given my commitment to provide you the latest information on the causes of and treatments for long COVID Brain Fog and Depression, today I am going to revisit how infectious diseases can cause psychiatric symptoms and share some infographics as to why SARS CoV-2 is one of the culprits, how it goes about damaging brain function, and how we can test for and treat the autoimmune diseases it can cause.
How Infections Cause Autoimmune Disease, and how SARS CoV-2 Plays a Role
Two world-renowned Israeli scientists have dubbed SARS CoV-2 “the autoimmune virus.” Back in 2020, in the early days of COVID, 16 different autoimmune diseases caused by this virus had already been identified. By 2021 five more autoimmune diseases had been reported. And as of 2022, 44% of patients with Long COVID had autoantibodies (antibodies attacking their own cells) in the bloodstream. Why is this happening?
A healthy immune system helps keep us alive by fending off viruses and bacteria while leaving the rest of our body intact. It does so by recognizing foreign proteins on the surface of these “bad bugs” and then attacking and destroying them. But sometimes our immune system can get confused and begin to attack our very cells. The reason is that proteins on the surfaces of our cells are identical to the proteins on the surfaces of the bugs. In the case of COVID, over two dozen proteins on the surface of the virus are identical to – they “mimic” - human cell proteins. It’s no wonder it’s been called the autoimmune virus!
Since these viral proteins are identical to our own, the immune system—especially in genetically vulnerable individuals who are prone to autoimmune conditions—is unable to distinguish “self” from “not self”, so it attacks both the proteins on the surface of the SARS virus as well as proteins on the surface of other human cells. This can affect our cognition, emotions and behaviors and ultimately lead to long COVID.
How Long COVID Causes Brain Fog and other Psychiatric Symptoms
The infographic below depicts the various causes of long COVID. In Section A, the virus first infects one’s nose, mouth, and respiratory system, which then starts an inflammation process that travels from the bloodstream to the brain. As we discussed in a prior blog, this inflammation then begins to damage our brain cells and the connections between them, resulting in disruptions of the circuits and systems in the brain that help determine mood, cognition, and behavior. This disruption then leads to depression, brain fog, cognitive impairment, anxiety, PTSD, and even psychosis.
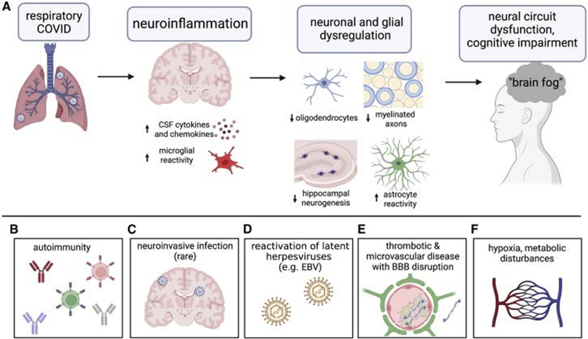
To visualize this damage better, consider what would happen if every wire in the electrical system in your house was suddenly overloaded by a lightning strike. All the wiring and the appliances connected to the electrical system would be damaged, or even destroyed, right? When chronic inflammation in our brains further develops into autoimmunity, the situation becomes even more complex. Antibodies begin to directly attack our brain cells, and the circuits and systems that help us think, feel, behave and live. In one sense, they attack the very fabric of our being! The good news is that we can diagnose that complexity and treat it. Please read on to learn what happens when our immune system attacks our brains, and how this condition can be evaluated and treated.
Brain Autoimmune Disease as a Root Cause of Psychiatric Symptoms
The infographic below depicts how our immune system can get confused by a virus like SARS CoV-2 and lose the ability to distinguish between the bacterial, viral or fungal infections on the one hand, and our brain cell receptors on the other, resulting in the production of antibodies that attack the brain. This process can result in some profound neuropsychiatric symptoms as shown in the yellow box, which are often treated with psychiatric medications alone. These medications can help bring some relief, and many psych meds have anti-inflammatory activity, but they don’t begin to alleviate the underlying root causes when antibodies are attacking brain cells. Fortunately, there is a way to diagnose and treat this type of brain-on-fire process—and at Potomac Psychiatry, in some patients we use a laboratory test called The Cunningham Panel.
The Cunningham Panel can Diagnose and Guide Treatment of Brain Autoimmune Disease
Dr. Madeleine Cunningham is a famous immunologist who has devoted her life’s work to researching brain autoimmunity at the University of Oklahoma. Dr. Cunningham researched and discovered the biomarker targets that indicate brain autoimmunity and the presence of anti-brain antibodies.
Dr. Craig Shimasaki, founder and CEO of Moleculera Labs, successfully translated Dr. Cunningham’s research into a clinical and commercial panel that bears her name, which is now available through their CLIA and COLA accredited clinical laboratory to the global scientific research and treating physicians’ communities. As a result of Dr. Shimasaki’s leadership, the Cunningham Panel has already benefited many thousands of patients and their loved ones, who had given up hope of ever getting better.
In his own words below, Dr. Shimasaki describes how the Cunningham Panel can point toward certain types of treatments that can neutralize the effects of the antibodies that attack the brain, and the exciting research findings that prove these treatments can bring about incredible life-altering results.
As Dr. Kehr has well described, a biological pathway called Molecular Mimicry is a common mechanism that leads to autoimmune syndromes in a genetically susceptible host. When infection-triggered autoimmune antibodies are generated and cross the blood brain barrier, they attack various targets in the brain resulting in a variety of neurologic, psychiatric, and behavioral symptoms that are often treated symptomatically with little or no improvement. Because most neurologic, psychiatric, and behavioral disorders are diagnosed and categorized by clinical symptoms, often these immune-mediated disorders are misdiagnosed in patients suffer for many years or decades before they are properly diagnosed and treated.
These syndromes are not new phenomena in children and adults. In 1686, Thomas Sydenham described a syndrome called “St. Vitus’ Dance” which is the result of a group A streptococcal (GAS) infection producing cross reactive antibodies against the basal ganglia resulting in abnormal movements and loss of fine-motor and emotional control. Certain parts of the GAS proteins such as the M protein shares sequence homology with human proteins in the heart and the basal ganglia in the brain, explaining why Sydenham chorea is the neurologic manifestation of Rheumatic Fever.
GAS has also been identified as the trigger for another condition known as PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection) and is one of many other infectious triggers in a syndrome known as PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). These disorders and syndromes are characterized by multiple symptoms including OCD, anxiety, restrictive eating disorders, motor and vocal tics and others.
The 5 serum biomarker targets in Moleculera Labs’ Autoimmune Encephalitis Panel (Cunningham Panel™) identify autoimmune antibodies directed against dopamine receptors, lysoganglioside GM1, tubulin, and their ability to stimulate calcium dependent calmodulin kinase II (CaMKII) in human neuronal cells. Watch Grace’s story to see how immune-mediated neuropsychiatric disorders can be diagnosed and treated with remarkable outcomes. For more information on the Moleculera panel targets and clinical performance measures read the 2020 Journal of Neuroimmunology article.
More recently, there have been case reports of SARS-Co-V2 associated with the onset of PANS in children illustrating that sequence homology of some part of the infection with targets in the human body may be the key requirement for immune-mediated autoimmune neuropsychiatric disorders.
Treating Long COVID Brain Fog and Depression through Root Cause Psychiatry
Dear Reader, if you or someone you love is suffering from long COVID, please don’t despair: dramatic daily breakthroughs are bringing new knowledge of how to diagnose and treat this condition, and new hope to those who suffer from it. Large, well-controlled scientific studies are well underway, and in the meantime many of us are sharing the results of our case reports (for example, my patient Tom) and smaller studies to help one another help our patients. It all comes down to determining the root causes that drive chronic illnesses, and treating them through Root Cause Psychiatry. And when our doctors find that a Cunningham Panel reveals antibodies to brain cells, symptom relief can often be brought about by adding immune system modulating medications (like IVIG or Rituximab) to psychiatric medications and talk therapy.
.png?width=144&height=144&name=Untitled%20design%20(34).png)



