Long COVID: The Brain Fog Pandemic
- Home
- Blog

Long COVID affects up to 30% of individuals who were previously infected. A variety of psychiatric symptoms can become chronic, including brain fog, depression, anxiety attacks, panic, and more. This blog will explain the root causes of long COVID symptoms, and how you can overcome them. You will learn:
- Long COVID, defined
- What causes long COVID
- The Connection Between Long COVID and Psychiatric Symptoms
- Treating COVID Brain Symptoms: Tom's Story
- Root Cause Psychiatry and Long COVID
Long COVID Brain: What is Long COVID?
Dear Reader, we are coming up on three years since the onset of COVID. For some, those years may feel like an eternity, particularly those known as “Long Haulers.” If you are suffering from long COVID or know of a friend or loved one with persisting symptoms, you realize how debilitating this condition can be. The medical term for long COVID is “Post-Acute Sequelae of COVID” (or PASC for short), and it is estimated that between 10-30% of people who tested positive have lingering symptoms beyond three months. Some long COVID patients have had 20 or more symptoms that persist, as this scourge can affect multiple organs and systems throughout the body. When it affects the brain, many patients report brain fog, depression, anxiety, and panic attacks—“long COVID brain”, in other words.
What Causes Long COVID?
Researchers are exploring a number of possible causes of long COVID, including persisting coronavirus infection, viral fragments that have not been cleared from cells, gut microbiome problems, chronic inflammation, mitochondrial malfunction (mitochondria are the cellular “power plants” that create energy to enable life itself), direct damage to tissue, blood clots in small arteries, autoimmunity (antibodies that attack both the virus and our own cells), immune system dysregulation, and reactivation of microbes “hiding out” in the body from prior infections (e.g. Lyme spirochetes, Epstein Barr virus, strep, etc.).
In a prior blog I discussed how these viruses and bacteria can trigger psychiatric symptoms such as cognitive problems (brain fog), post-traumatic stress disorder (PTSD), depression, anxiety including obsessive-compulsive disorder (OCD), mental fatigue, and even psychosis. In this blog we will focus on why Coronavirus SARS-CoV-2 is one such culprit.
Long COVID Psychiatric Symptoms
In our practice, and reported by colleagues elsewhere, following a COVID infection there are a number of patients presenting with psychiatric symptoms for the first time, as well as previously stabilized patients that had dramatic worsening of their symptoms. Long COVID’s psychiatric manifestations can include brain fog and other cognitive problems, persisting fatigue, depression with an inability to experience pleasure, anxiety, as well as other disturbances such as psychosis, suicidal feelings, OCD, PTSD, and insomnia.
How Does the Coronavirus Cause Psychiatric Symptoms?
Emerging scientific evidence suggests that SARS-CoV-2 affects the brain in a number of ways. Although somewhat rare, the virus can infect the brain itself, which can be associated with movement disorders, stroke, and other neurological disorders. This is more likely with those patients who are hospitalized, where 21% show signs of brain infection on brain imaging tests. What is far more common, particularly among patients with mild to moderate symptoms of COVID, is chronic brain inflammation resulting from prolonged immune system activity. Below is an infographic I will use to explain what happens. At the top is a blood vessel feeding the brain, and below the vessel are four types of brain cells:
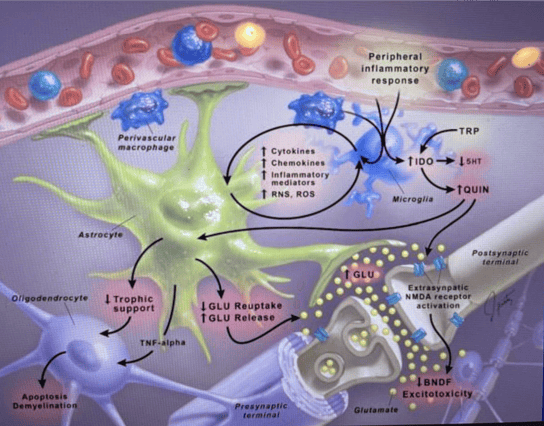
- The microglia (in blue) – there are one trillion microglia in your brain, and they are the brain’s immune system cells
- Astrocytes (in green) – these are the “nurturing cells” in the brain that support, nourish and protect all the other cells
- Oligodendrocytes (in purple) – these important cells lay down and repair the myelin sheaths – the insulation surrounding neurons – to keep firing neurons from “short-circuiting” one another
- Neurons and their synapses (purple myelin surrounding white cells) – probably already familiar to you, there are “only” 100 billion neurons in your brain, which communicate with one another across one thousand trillion synapses in circuits that help create emotions, thoughts, and behaviors.
Keeping in mind the infographic above, here’s how chronic brain inflammation develops. As your body’s immune system fights the coronavirus, inflammatory molecules like IL6 and TNF Alpha travel through the blood vessels, and then cross from the bloodstream through the blood-brain barrier into the brain. Once inside, they signal to the microglia that “uh-oh, there’s an infection coming.” The microglia then ramp-up their metabolism, change their physical form into a “warrior state,” and begin to release all sorts of signaling molecules into the surrounding tissues like free radicals. These molecules then attract white blood cells to enter the brain from the bloodstream (like the two “perivascular macrophages”seen above, also in blue). This is part of the normal acute inflammation process needed to kill off viruses that invade the brain. But what happens when it becomes chronic inflammation? Here’s where long COVID begins to develop.
Macrophage is translated as “big eater.” They and the microglia start “eating” what is around them, damaging the astrocytes which stop nourishing and start releasing excessive amounts of glutamate (a toxic neurotransmitter). This causes the oligodendrocytes to self-destruct, so they can no longer repair the myelin insulation surrounding the neurons. Without their support systems in place to protect them, those poor neurons and synapses get battered by the inflammation and oxidative stress. They lose their “BDNF fertilizer” and not only become damaged, but in extreme cases even healthy neurons get gobbled up by the microglia. This damaging cycle perpetuates itself, resulting in the long COVID psychiatric symptoms mentioned above.
Treating COVID Brain Symptoms: Tom's Story
Tom was a 20 year old college student who presented with brain fog, depression, anxiety, fatigue, panic attacks and gut symptoms including gas, bloating, diarrhea and abdominal pain. All of these symptoms followed his COVID infection a year earlier. He had already seen a couple of psychiatrists, and had been prescribed medications, but hadn’t improved. He felt hopeless, had trouble meeting the demands of daily life, and just wanted his old life back.
To help evaluate and treat Tom’s debilitating condition, we enrolled him in our Root Cause Psychiatry Program, where we implemented a variety of diagnostic tests. In Long COVID patients, these may include:
- A genetic test through a simple cheek swab which helps us more precisely prescribe a medication to help alleviate the symptoms of brain fog, depression or anxiety.
- A microbiome stool test, as 70% of our body’s immune system resides in the gut, and healing the gut improves the immune system dysregulation behind long-COVID.
- A test of cellular health that helps us create a nutritional psychiatry approach to improve cellular energy production, and repair damage caused by inflammation
- A cytokine panel, IncellKINE, that looks at inflammatory chemicals in the blood, and uses Artificial Intelligence to recommend targeted medications to reduce their numbers
- A test that measures antibodies that attack brain cells, The Cunningham Panel, leading to recommendations for immunotherapy, which is generally combined with psychiatric medication
Tests for other viruses or bacteria that co-infect, or are reactivated from prior infections, like Lyme, Strep, Herpes, and others
How We Treated Tom’s Long COVID Depression, Anxiety and Brain Fog
Based upon Tom’s symptoms and genetic testing results, we began him on the antidepressant Trintellix, which treats depression and also has numerous immune system modulating effects; and a methylation support product (good methylation is essential for a healthy immune system), which helped him improve about 50% after one month. He was found to have gut inflammation (caused largely by gluten intolerance), leaky gut syndrome, and cellular mitochondrial dysfunction, so our functional nutritionist, Julie Wendt, began him on a regimen of nutrients, supplements, and a gut-healing protocol. After about three additional months these interventions brought about a 70% recovery. Based upon the results of his cytokine and anti-brain antibody panels, we referred him to an immunology group who then added an immune modulating medication, Rituximab, to the interventions we had initiated. This combined approach achieved a 90% recovery five months later. After nine months of treatment Tom entered CBT therapy to reframe the trauma caused by his COVID, and we are optimistic that he will have a full recovery.
Learn More About How Our Root Cause Psychiatry Program Treats Long COVID
If you or someone you love may be suffering from emotional or cognitive symptoms from Long COVID, including brain fog, depression, anxiety, panic attacks or psychosis, contact us for a no-cost, 15-minute consultation with Dr. Bruce Kehr or Dr. Margery Johnson, along with our functional nutritionist, Julie Wendt. To schedule your consultation, please email Dana Schwartz at dana.schwartz@potomacpsychiatry.com, or call 301-984-9791.
.png?width=144&height=144&name=Untitled%20design%20(34).png)