Navigating Treatment Resistance in Psychiatry: A Holistic Approach
- Home
- Blog
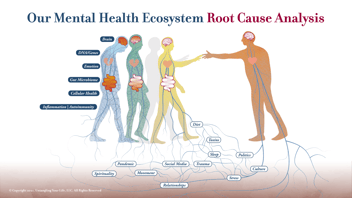
"What is it called when medication doesn't work?" This question, frequently asked by psychiatric patients, touches the heart of a challenging and complex issue in mental health care: treatment resistance. In psychiatric terms, we often refer to this as "treatment-resistant depression," "treatment-resistant schizophrenia," or "treatment-resistant bipolar disorder," among others. At Potomac Psychiatry, our approach to these seemingly intractable conditions is deeply rooted in our comprehensive Root Cause Psychiatry™ philosophy.
Understanding Treatment Resistance
Treatment resistance occurs when a patient does not respond adequately to standard treatments for their diagnosed mental health condition. This can manifest as a lack of improvement in symptoms or only partial relief, even after trying multiple medications or therapies. It's a situation that can be deeply frustrating and disheartening for patients and clinicians alike.
The Root Cause Psychiatry™ Philosophy: A Deeper Dive
Our evaluation and treatment philosophy doesn't just look at symptoms; we delve deeper to understand the underlying root causes of treatment resistance. We take a holistic and comprehensive approach, considering the full spectrum of potential contributing factors. Through a variety of standardized tests, and a comprehensive team-based approach, we can look at the underlying root cause drivers of chronic mental health conditions. Our goal is to ensure that our diagnostic process is all-encompassing, leaving no stone unturned in our pursuit to identify and address every possible root cause of treatment resistance.
- Misdiagnosis and Medication Issues: Sometimes, the problem starts with a misdiagnosis or incorrect medication choices and dosages. Ensuring an accurate diagnosis and appropriate medication management is our first step. This typically involves the use of pharmacogenetic testing to understand the interactions between the patient’s personal genome and specific medications.
- Underlying Medical Conditions: We explore underlying medical conditions that may be contributing to psychiatric symptoms. Conditions like sleep apnea syndrome, thyroid disorders, or reactivated viral infections, including long COVID, can significantly impact mental health.
- Genetic Factors: Understanding how to upregulate or downregulate genes that predispose individuals to worsening psychiatric conditions is vital. Genetic testing, including pharmacogenomics testing by Genomind, and mental wellness and brain optimization genetic testing provided by IntellxxDNA, can guide us in personalizing treatment plans.
- Gut Microbiome and Digestive Health: The gut-brain axis plays a crucial role in mental health. Dysbiosis, inflammation, maldigestion, malabsorption, pathogenic bacteria, and leaky gut syndrome can all contribute to psychiatric symptoms. Addressing gut health is often a key component of our treatment strategy.
- Micronutrient Deficiencies: We assess for and address micronutrient deficiencies, such as vitamin and mineral deficiencies, which can have a significant impact on brain function and mental health.
- Immune System Dysregulation: Chronic autoinflammation, autoimmunity, and antibodies to brain tissue following infections like Lyme and other tickborne diseases, strep, COVID, or EBV virus/mononucleosis are evaluated as potential contributors to psychiatric symptoms.
- Food Sensitivities: We also consider food sensitivities, which can exacerbate mental health conditions.
- Environmental Factors: The presence of psychiatric symptoms and heavy metals, exposure to pesticides, and the insidious role of mycotoxins and mental disorders are critical pieces of this puzzle. At Potomac Psychiatry, we understand that these environmental toxins can profoundly impact mental health, potentially leading to or exacerbating treatment-resistant conditions.
Our Approach to Treatment
Our treatment approach is as unique as the individual patient. We use a combination of evidence-based psychiatric treatments, lifestyle modifications, nutritional interventions, and when necessary, referral to other medical specialists for comprehensive care. All of these interventions are based on specific genetic and other laboratory test findings that are unique to the patient. We call this our “N of One” approach.
Psychotherapy and Medication Optimization: We combine psychotherapy with careful medication management, tailored to the individual's genetic profile and specific condition.
Lifestyle Interventions: Lifestyle changes, including sleep hygiene, exercise, and stress reduction techniques, are integrated into our treatment plans.
Nutritional Therapy: We focus on dietary changes and supplements to address gut health issues and nutritional deficiencies.
Collaborative Care: Collaborating with other healthcare professionals, for example endocrinologists, immunologists, and infectious disease specialists, ensures a comprehensive approach to treating underlying medical conditions that may be contributing to psychiatric symptoms.
Empowering Patients: Education and empowerment are key. We believe in involving patients in their treatment plans, ensuring they understand the why and how of each intervention.
Conclusion
In summary, treatment resistance in psychiatry is a multifaceted issue that demands a comprehensive and holistic approach. At Potomac Psychiatry, we are committed to exploring and addressing the root causes of each patient’s unique mental health challenges. Through our Root Cause Psychiatry™ Program, Autism Program, ReCODE/PreCODE, and Long COVID Depression and Brain Fog Programs, we offer hopeful and effective solutions to those struggling with treatment-resistant conditions, paving the way for healing and recovery.
Remember, treatment resistance is not the end of the road; it's a call to explore the underlying root causes at a deeper level, and at Potomac Psychiatry, we are here to guide you on that journey.
Whatever it Takes
To learn more and schedule a 15 minute No-Cost Consultation, click the button below.
.png?width=144&height=144&name=Untitled%20design%20(34).png)

.jpeg?width=352&name=AdobeStock_517132756%20(1).jpeg)