Marissa's 12-Month Journey in Our Root Cause Psychiatry Program
- Home
- Blog

Marissa was a 45-year-old IT executive and mother of three. Before she entered our Root Cause Psychiatry program, she had been treated by several other psychiatrists, prescribed a number of different antidepressants and antianxiety medications, and had undergone two trials of psychotherapy—yet despite these interventions, her mental health continued to deteriorate. Her anger and rage attacks, directed at her husband and children, were worsening to the point that they no longer wanted to be in her company. Recently, she had begun to direct her blowups toward colleagues at work as well. Scared she might lose everything, Marissa came to us feeling desperate and hopeless, yet also suspicious and cynical that any further intervention could improve her situation. This was fully understandable—thus far, the field of psychiatry had failed her.
As a child, Marissa had suffered from mild depression and anxiety. While growing up in a small southern town, she was bullied at school for her shyness, scorned because she was always at the top of her class, and was portrayed as a “kiss up” to the teachers by her peers. To make matters worse, at age nineteen she was date raped. Despite these traumatic experiences, she went on to graduate college magna cum laude, and subsequently graduated with honors from a prestigious university with a master’s degree in computer science. Her home life stabilized for a number of years after that, and despite the stress of a high-level executive position, she had been reasonably content with her relatively joyless life. However, four years ago, after she was involved in a serious motor vehicle accident in which she had sustained a concussion, things began to devolve.
Marissa began suffering from mood swings, irritability, temper outbursts, trouble sustaining focus, executive dysfunction, insomnia, and occasional “spells” where she didn’t feel like herself and felt quite out of sorts, including a number of unusual sensory experiences. She tried to manage her mood, anxiety, and cognitive symptoms with a diet and lifestyle approach that would be considered healthy by most standards. Despite her consistent exercise and a diet that included fruits and vegetables, her emotional symptoms were just getting worse; she had also developed gastrointestinal symptoms including bloating, gas, cramping, and alternating periods of constipation and loose stools. To make matters worse, Marissa came down with COVID in 2021, and while she had a relatively mild course of illness, she complained of persisting brain fog. There was a family history of autoimmune diseases, and Marissa had persisting muscle aches and joint pains following her COVID infection.
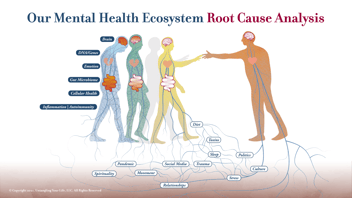
Her prior psychiatrists had focused on treating her symptoms, having diagnosed her with bipolar disorder and ADHD. But they neglected to search for the root causes of her serious emotional illness. This is why Marissa came to us for help. After her initial consultation with our team, she started our 12-month Root Cause program in July of 2021. Her journey through the program recently ended, and the results have made a meaningful impact on her life. Below is a synopsis of how this journey progressed over the course of a year.
Months 1-3
After gathering a comprehensive history for Marissa, Dr. Kehr and Julie ordered a number of diagnostic tests. These first two steps of our Root Cause program enable our team to begin to understand and uncover the root causes of our patient’s distress—and Marissa’s results were very clarifying.
Marissa’s initial genetic test revealed a number of explanations for her childhood and adult symptoms of joylessness. There was a methylation problem, due to a 70% decline in MTHFR enzyme activity. To address this genetic vulnerability, we began her on a methylation support product, Enlyte, which helped to boost her production of serotonin, norepinephrine, dopamine, and glutathione (a powerful brain antioxidant); and reduce her production of glutamate (an “excitotoxic” neurotransmitter). Her COMT genetic variant broke down dopamine (the feel-good neurotransmitter) too rapidly, so we put her on a green tea extract to boost dopamine and help address her trouble sustaining attention and executive dysfunction. Her CACNA1C variant revealed increased brain cell firing rates, which predisposes to depression, anxiety, and trouble keeping an even mood. To block this genetic effect we started Marissa on omega 3 supplements and magnesium threonate (the form of magnesium that enters the brain). Her MRI and EEG tests were normal. She was diagnosed with sleep apnea syndrome, however, and began CPAP treatment. Dr. Kehr also continued prescribing her antidepressant, Trintellix.
Meanwhile, Julie ordered tests to assess the health of Marissa’s gut microbiome and cellular functions. The microbiome testing revealed infection, dysbiosis, and metabolic imbalances; and possible SIBO. Marissa began Julie’s initial nutrition plan based on these findings. Julie also began her on Ashwagandha, a supplement to calm her overactive adrenal gland, which was pumping out too much cortisol and adrenaline.
These initial interventions took place over the course of the first three months of our program. By the end of the third month, Marissa reported some modest improvement in symptoms.
Months 4-6
Over the next three months of Marissa’s program, we ordered some additional tests to further refine our diagnostic thinking and treatment approach. A diagnosis of SIBO (small intestine bacterial overgrowth) was confirmed by a breath test. At Julie’s recommendation she began taking Candibactin and Allimax, and was prescribed a Mediterranean Diet that was customized to her food preferences. A test of cellular functioning revealed elevated levels of mitochondrial dysfunction, inflammation, omega 3 imbalances, oxidative stress, and methylation problems. These were addressed with supplements that supported mitochondrial function, increased doses of omega 3 fatty acids, and intermittent fasting combined with an exercise program. She also started what is called an “SPM” (a Specialized Pro-Resolving Modulator), a supplement that would dampen her excessive immune system response which was fueling chronic inflammation.
Marissa was also encouraged to meditate. We frequently recommend “prescription meditation” at Potomac Psychiatry, as meditation boosts immune system functioning, reduces inflammation, and “turns on” a number of genes that promote mental health, including BDNF, the “brain’s fertilizer.”
These root cause findings, followed by targeted interventions to address each root cause, began to improve Marissa’s gut symptoms, energy level, and brain fog. In our mental health ecosystem, the mind-body connection is a powerful determinant of mental wellness or illness, and while much progress had been made on improving her physical symptoms, her ability to manage her emotions had only partially responded. We would target this during the next phase of our program.
Months 7-12
Given that substantial improvement remained elusive, despite these interventions, Dr. Kehr began to focus on potential residual effects of her concussion. A detailed review of neurologic symptoms pointed toward the possibility of partial complex seizures. He ordered a number of tests to assess and treat a possible post-concussion syndrome and seizure disorder. These included an FDG PET scan, an anti-brain antibody test, a genetic test focused on brain optimization, and a blood panel for inflammatory cytokines. The PET scan revealed areas of her temporal lobe that had low metabolism, which was consistent with the head injury symptoms and partial complex seizures. The blood panel revealed a number of elevations of inflammation markers, and the genetic test revealed a numerous genes that would accelerate inflammation in her body and brain. Finally, another blood study revealed high levels of anti-brain antibodies, an autoimmune disease known as an autoimmune encephalopathy.
As a result of these findings, Dr. Kehr began Marissa on Lyrica (pregabalin), which has anti-inflammatory, anticonvulsant, mood stabilizing, and anti-anxiety properties. Not only was Lyrica capable of slowing down Marissa’s over-active immune system, it also would turn off the overactivity in her brain by blocking the excessive activity of her CACNA1C gene. He also added Ritalin (Methylphenidate ER) to the regimen to help with her brain fog, attention deficits, and executive functioning. In addition, he prescribed intravenous infusions of ketamine and glutathione to further reduce brain inflammation and oxidative stress and reduce the destructive effects of the antibodies that were attacking Marissa’s brain cells.
Two months later, Marissa reported a significant improvement, and the ketamine treatments were reduced to once a month. She reported feeling better than she had for many years, but she was not completely out of the woods. Our goal with our Root Cause program is to help patients feel whole, achieving a full recovery. Because of persisting mood swings and temper outbursts, and elevated antibodies to brain tissue, we referred Marissa for immunologic therapy to rebalance her immune system and improve her brain function; she was also started on rituximab and responded really well. At this point she finally had enough mental energy and emotional reserve to enter talk therapy with Dr. Kehr to deal with her longstanding issues related to unresolved trauma—this step underscored the substantial progress she had made toward our program goal.
Marissa’s story illustrates the core principle of our Root Cause Psychiatry program: patient, persistent efforts to uncover the root causes that drive emotional and behavioral problems, followed by systematically addressing each and every one with targeted interventions, can bring about recovery from a chronic mental health condition that was previously resistant to treatment.
On average, patients like Marissa typically show some improvement by Month 3, additional improvement by Month 6, and substantial improvement by Month 12. It takes that long to reverse complex genetic, epigenetic, cellular, immunologic, and gut microbiome-related problems to feel well and restore health. She had the courage to stay the course throughout those first twelve months and was rewarded for her persistence with a tangible turnaround in her mental health. Her family was grateful, and Julie, Dana, and I shared virtual high-fives.
.png?width=144&height=144&name=Untitled%20design%20(34).png)